Amnesia is a condition in which memory is disturbed or lost. The causes of amnesia have traditionally been divided into categories. Functional causes are psychological factors, such as mental disorder, post-traumatic stress or, in psychoanalytic terms, defense mechanisms. Amnesia may also appear as spontaneous episodes, in the case of transient global amnesia.
Forms of amnesia
Anterograde amnesia, is the loss of short-term memory, the loss or impairment of the ability to form new memories through memorization. Persons may find themselves constantly forgetting information, people or events after a few seconds or minutes, because the data does not transfer successfully from their conscious short-term memory into permanent long-term memory.
Retrograde amnesia, the loss of pre-existing memories to conscious recollection, beyond an ordinary degree of forgetfulness. The person may be able to memorize new things that occur after the onset of amnesia (unlike in anterograde amnesia), but is unable to recall some or all of their life or identity prior to the onset.
However, there are different types of memory, for example procedural memory (i.e. automated skills) and declarative memory (personal episodes or abstract facts), and often only one type is impaired. For example, a person may forget the details of personal identity, but still retain a learned skill such as the ability to play the piano.
In addition, the terms are used to categorize patterns of symptoms rather than to indicate a particular cause (etiology). Both categories of amnesia can occur together in the same patient, and commonly result from drug effects or damage to the brain regions most closely associated with episodic memory: the medial temporal lobes and especially the hippocampus.
An example of mixed retrograde and anterograde amnesia may be a motorcyclist unable to recall driving his motorbike prior to his head injury (retrograde amnesia), nor can he recall the hospital ward where he is told he had conversations with family over the next two days (anterograde amnesia).
The effects of amnesia can last long after the condition has passed. Some sufferers claim that their amnesia changes from a neurological condition to also being a psychological condition, whereby they lose confidence and faith in their own memory and accounts of past events.
Another effect of some forms of amnesia may be impaired ability to imagine future events. A 2006 study showed that future experiences imagined by amnesiacs with bilaterally damaged hippocampus lacked spatial coherence, and the authors speculated that the hippocampus may bind different elements of experience together in the process of re-experiencing the past or imagining the future.
Types and causes of amnesia
Post-traumatic amnesia is generally due to a head injury (e.g., a fall, a knock on the head). Traumatic amnesia is often transient, but may be permanent of either anterograde, retrograde, or mixed type. The extent of the period covered by the amnesia is related to the degree of injury and may give an indication of the prognosis for recovery of other functions. Mild trauma, such as a car accident that results in no more than mild whiplash, might cause the occupant of a car to have no memory of the moments just before the accident due to a brief interruption in the short/long-term memory transfer mechanism. The sufferer may also lose knowledge of who people are.
Dissociative amnesia results from a psychological cause as opposed to direct damage to the brain caused by head injury, physical trauma or disease, which is known as organic amnesia. Dissociative amnesia can include:
- Repressed memory refers to the inability to recall information, usually about stressful or traumatic events in persons’ lives, such as a violent attack or rape. The memory is stored in long term memory, but access to it is impaired because of psychological defense mechanisms. Persons retain the capacity to learn new information and there may be some later partial or complete recovery of memory. This contrasts with e.g. anterograde amnesia caused by amnestics such as benzodiazepines or alcohol, where an experience was prevented from being transferred from temporary to permanent memory storage: it will never be recovered, because it was never stored in the first place. Formerly known as “Psychogenic Amnesia”.
- Dissociative Fugue (formerly Psychogenic Fugue) is also known as fugue state. It is caused by psychological trauma and is usually temporary, unresolved and therefore may return. The Merck Manual defines it as “one or more episodes of amnesia in which the inability to recall some or all of one’s past and either the loss of one’s identity or the formation of a new identity occur with sudden, unexpected, purposeful travel away from home.” While popular in fiction, it is extremely rare.
- Posthypnotic amnesia is where events during hypnosis are forgotten, or where past memories are unable to be recalled.
- Lacunar amnesia is the loss of memory about one specific event.
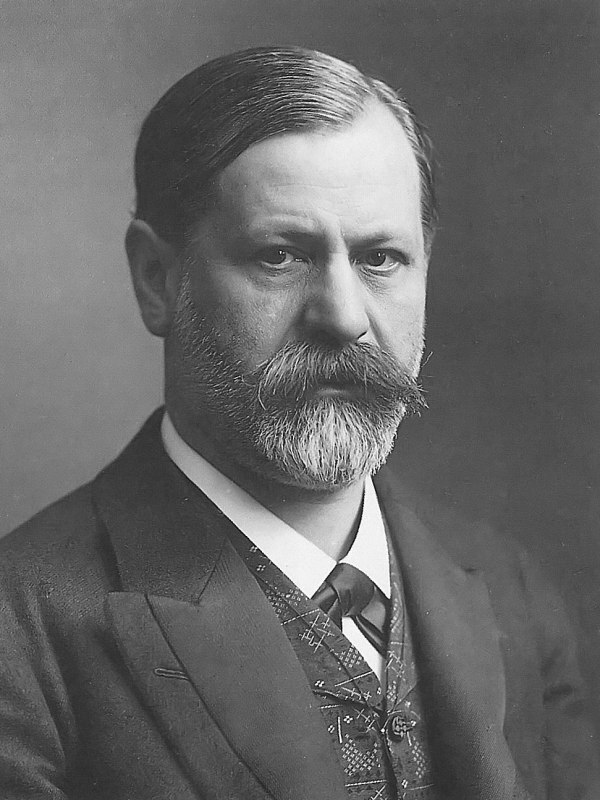
- Childhood amnesia (also known as infantile amnesia) is the common inability to remember events from one’s own childhood. Sigmund Freud notoriously attributed this to sexual repression, while modern scientific approaches generally attribute it to aspects of brain development or developmental psychology, including language development
- Transient global amnesia is a well-described medical and clinical phenomenon. This form of amnesia is distinct in that abnormalities in the hippocampus can sometimes be visualized using a special form of magnetic resonance imaging of the brain known as diffusion-weighted imaging (DWI). Symptoms typically last for less than a day and there is often no clear precipitating factor nor any other neurological deficits. The cause of this syndrome is not clear, hypotheses include transient reduced blood flow, possible seizure or an atypical type of migraine. Patients are typically amnestic of events more than a few minutes in the past, though immediate recall is usually preserved.
- Source amnesia is a memory disorder in which someone can recall certain information, but they do not know where or how they obtained the information.
- Memory distrust syndrome is a term invented by the psychologist Gisli Gudjonsson to describe a situation where someone is unable to trust their own memory.
- Blackout phenomenon can be caused by excessive short-term alcohol consumption, with the amnesia being of the anterograde type.
- Korsakoff’s syndrome can result from long-term alcoholism or malnutrition. It is caused by brain damage due to a vitamin B1 deficiency and will be progressive if alcohol intake and nutrition pattern are not modified. Other neurological problems are likely to be present in combination with this type of Amnesia. Korsakoff’s syndrome is also known to be connected with confabulation.
- Drug-induced amnesia is intentionally caused by injection of an amnesiac drug to help a patient forget surgery or medical procedures, particularly those not performed under full anesthesia, or likely to be particularly traumatic. Such drugs are also referred to as “premedicants.” Most commonly a 2′-halogenated benzodiazepine such as midazolam or flunitrazepam is the drug of choice, although other strongly amnestic drugs such as propofol or scopolamine may also be used for this application. Memories of the short time frame in which the procedure was performed are permanently lost or at least substantially reduced, but once the drug wears off, memory is no longer affected.
- Electroconvulsive therapy in which seizures are electrically induced in patients for therapeutic effect can have acute effects including both retrograde and anterograde amnesia.
- Prosopamnesia is the inability to remember faces, even in the presence of intact facial recognition capabilities. Both acquired and inborn cases have been documented.
- Situation-Specific amnesia can arise in a variety of circumstances (e.g., committing an offence, child sexual abuse) resulting in PTSD. It has been claimed that it involves a narrowing of consciousness with attention focused on central perceptual details and/or that the emotional or traumatic events are processed differently from ordinary memories.
Types of Amnesia
Post-traumatic amnesia
Post-traumatic amnesia (PTA) is a state of confusion that occurs immediately following a traumatic brain injury (TBI) in which the injured person is disoriented and unable to remember events that occur after the injury. The person may be unable to state his or her name, where he or she is, and what time it is. When continuous memory returns, PTA is considered to have resolved. While PTA lasts, new events cannot be stored in the memory. About a third of patients with mild head injury are reported to have “islands of memory”, in which the patient can recall only some events. During PTA, the patient’s consciousness is “clouded”. Because PTA involves confusion in addition to the memory loss typical of amnesia, the term “posttraumatic confusional state” has been proposed as an alternative.
There are two types of amnesia: retrograde amnesia (loss of memories that were formed shortly before the injury) and anterograde amnesia (problems with creating new memories after the injury has taken place). Both retrograde and anterograde forms may be referred to as PTA, or the term may be used to refer only to anterograde amnesia.
Frequently the last symptom to ameliorate after a loss of consciousness, anterograde amnesia may not develop until hours after the injury. A common example in sports concussion is the quarterback who was able to conduct the complicated mental tasks of leading a football team after a concussion, but has no recollection the next day of the part of the game that took place after the injury. Retrograde amnesia sufferers may partially regain memory later, but memories are not regained with anterograde amnesia because they were not encoded properly.
The term “posttraumatic amnesia” was first used in 1928 in a paper by Symonds to refer to the period between the injury and the return of full, continuous memory, including any time during which the patient was unconscious.
Measure of traumatic brain injury severity
TBI severity using PTA
Severity PTA
Very mild < 5 minutes
Mild 5–60 minutes
Moderate 1–24 hours
Severe 1–7 days
Very severe 1–4 weeks
Extremely severe > 4 weeks
PTA has been proposed to be the best measure of head trauma severity, but it may not be a reliable indicator of outcome. However, PTA duration may be linked to the likelihood that psychiatric and behavioral problems will occur as consequences of TBI.
Classification systems for determining the severity of TBI may use duration of PTA alone or with other factors such as Glasgow Coma Scale (GCS) score and duration of loss of consciousness (LOC) to divide TBI into categories of mild, moderate, and severe. One common system using all three factors and one using PTA alone are shown in the tables at right. Duration of PTA usually correlates well with GCS and usually lasts about four times longer than unconsciousness.
PTA is considered a hallmark of concussion, and is used as a measure of predicting its severity, for example in concussion grading scales. It may be more reliable for determining severity of concussion than GCS because the latter may not be sensitive enough; concussion sufferers often quickly regain a GCS score of 15.
Longer periods of amnesia or loss of consciousness immediately after the injury may indicate longer recovery times from residual symptoms from concussion. Increased duration of PTA is associated with a heightened risk for TBI complications such as post-traumatic epilepsy.
Duration of PTA may be difficult to gauge accurately; it may be overestimated (for example, if the patient is asleep or under the influence of drugs or alcohol for part of the time) or underestimated (for example, if some memories come back before continuous memory is regained). The Galveston Orientation and Amnesia Test (GOAT) exists to determine how oriented a patient is and how much material they are able to recall.
Psychogenic amnesia
Psychogenic amnesia, also known as functional amnesia or dissociative amnesia, is a memory disorder characterized by extreme memory loss that is caused by extensive psychological stress and that cannot be attributed to a known neurobiological cause. Psychogenic amnesia is defined by (a) the presence of retrograde amnesia (the inability to retrieve stored memories leading up to the onset of amnesia), and (b) an absence of anterograde amnesia (the inability to form new long term memories). Dissociative amnesia is due to psychological rather than physiological causes and can sometimes be helped by therapy.
There are two types of psychogenic amnesia, global and situation-specific. Global amnesia, also known as fugue state, refers to a sudden loss of personal identity that lasts a few hours to days, and is typically preceded by severe stress and/or depressed mood. Fugue state is very rare, and usually resolves over time, often helped by therapy. In most cases, patients lose their autobiographical memory and personal identity even though they are able to learn new information and perform everyday functions normally. Other times, there may be a loss of basic semantic knowledge and procedural skills such as reading and writing. Situation-specific amnesia occurs as a result of a severely stressful event, as in post-traumatic stress disorder, child sex abuse, military combat or witnessing a family member’s murder or suicide, and is somewhat common in cases of severe and/or repeated trauma.
Memory and the brain
Overview
There are three types of memory – sensory, short-term, and long-term memory. Sensory memory lasts up to hundreds of milliseconds; short-term memory lasts from seconds to minutes; while anything else longer than short-term memory is considered to be a long-term memory.
Information obtained from the peripheral nervous system (PNS) is processed in four stages – encoding, consolidating, storage, and retrieval. During encoding, the limbic system is responsible for “bottlenecking” or filtering information obtained from the PNS. According to the type of information being processed in a given instance, the duration of consolidating stage varies drastically. The majority of consolidated information gets stored in the cerebral cortical networks where the limbic system record episodic-autobiographical events. These stored episodic and semantic memories can be obtained by triggering the uncinate fascicle that interconnects the regions of the temporofrontal junction area.
Emotion seems to play an important role in memory processing in structures like the cingulated gyrus, the septal nuclei, and the amygdala that is primarily involved in emotional memories. Functional imaging of normal patients reveal that right-hemisperic amygdala and ventral prefrontal regions are activated when they were retrieving autobiographical information and events. Additionally, the hippocampal region is known to be linked to recognizing faces.
Researchers have found that emotional memories can be suppressed in non-mentally ill individuals via the prefrontal cortex in two stages – an initial suppression of the sensory aspects of the memory, followed by a suppression of the emotional aspect. It has also been proposed that glucocorticoids can impair memory retrieval; rats and human males have been shown to be affected by this mechanism.
Traumas can interfere with several memory functions. Dr. Bessel van der Kolk divided these functional disturbances into four sets: traumatic amnesia, global memory impairment, dissociative processes and traumatic memories’ sensorimotor organization. Traumatic amnesia involves the loss of remembering traumatic experiences. The younger the subject and the longer the traumatic event is, the greater the chance of significant amnesia. Global memory impairment makes it difficult for these subjects to construct an accurate account of their present and past history. Dissociation refers to memories being stored as fragments and not as unitary wholes. Not being able to integrate traumatic memories seems to be the main element which leads to PTSD. In the sensorimotor organization of traumatic memories, sensations are fragmented into different sensory components.
Comparison with organic causes
Clinically, psychogenic amnesia is characterized by the loss of the ability to retrieve stored memory without any apparent neurological damage; while organic amnesia is characterized by damages to the medial or anterior temporal and/or prefrontal regions caused by stroke, traumatic brain injury, ischemia, and encephalitis. Some characteristics that define organic amnesia is the maintenance of personal identity, basic semantic knowledge and procedural skills as well as neuroradiological images showing cerebral damage to the cortical and/or subcortical areas known to be associated with long-term memory while some characteristics that define psychogenic amnesia is the loss of personal identity, semantic knowledge, and procedural abilities at least in the early phase of amnesia as well as damage directly affecting cerebral areas critical for memory functioning that cannot be detected in clinical history or neuroradiological exams.
Imaging
Psychogenic amnesia is defined by the lack of structural damage to the brain, but upon functional imaging, an abnormal brain activity can be seen. Tests using functional magnetic resonance imaging suggest that patients with psychogenic amnesia are unable to retrieve emotional memories normally during the amnesic period, suggesting that changes in the limbic functions are related to the symptoms of psychogenic amnesia. By performing a positron emission tomography activation study on psychogenic amnesic patients with face recognition, it was found that activation of the right anterior medial temporal region including the amygdala was increased in the patient whereas bilateral hippocampal regions increased only in the control subjects, demonstrating again that limbic and limbic-cortical functions are related to the symptoms of psychogenic amnesia.
Risk factors
Patients exposed to physically or emotionally traumatic events are at a higher risk for developing psychogenic amnesia because they seem to have damaged the neurons in the brain. Examples of individuals at greater risk of psychogenic amnesia due to traumatic events include soldiers who have experienced combat, individuals sexually and physically abused during childhood and individuals who have experienced domestic violence, natural disasters, or terrorist acts; essentially any sufficiently severe psychological stress, internal conflict, or intolerable life situation. Child abuse, especially chronic child abuse starting at an early age has been related to the development of high levels of dissociative symptoms, including amnesia for abuse memories. The study strongly suggested that “independent corroboration of recovered memories of abuse is often present” and that the recovery of the abuse memories generally is not associated with psychotherapy.
Prevalence
Elliot’s study of a randomized nationwide sample (n=505) found that situation-specific psychogenic amnesia was somewhat common in the general population. 72% of subjects reported a profoundly distressing emotional trauma; 32% of these reported amnesia about part or all of the trauma, followed by “delayed recall” of the event. Traumatic events most commonly associated with psychogenic amnesia were witnessing a suicide or murder, and being sexually abused. Elliott also found that psychogenic amnesia was most strongly associated with severe and/or repeated traumas, and with traumas during childhood. When encountering stimuli similar to the trauma(s), subjects often reported many episodes of dissociation prior to the delayed recall. The most common “trigger” for recalling the traumatic event was a media event (e.g., while watching television or a movie), the least common trigger was psychotherapy or counseling.
Several studies have found that situation-specific psychogenic amnesia is common in verified victims of severe child abuse:
- In a 1994 study, Williams found that amongst women with confirmed histories of childhood sexual abuse, about one third of subjects did not recall the abuse during interviews as adults; because these same women were usually willing to discuss other potentially embarrassing or shameful incidents (e.g, abortions, prostitution, sexual assaults as adults) Williams concluded the women had genuinely lost access to the traumatic memories. In a follow-up study published the next year, Williams found that in women (n=129)with documented histories of childhood sexual abuse, 16% reported a period when they were unable to recall all or part of the abuse.
Widom and Morris found that in adults (n=450) with confirmed childhood histories of severe neglect and abuse (physical and/or sexual), 59.3% reported periods of partial or complete amnesia for the maltreatment. Amnesia for abuse was most associated with cases of multiple perpetrators and fears of death if the abuse was disclosed. - Dahlenberg studied 17 women who recovered memories of childhood sexual abuse while in therapy; six independent evaluators determined that all 17 women adequately corroborated the memories.
Theoretical explanations
Psychogenic amnesia is far from being completely understood and while several explanations have been proposed, none of them have been verified as the mechanism that fits all types of psychogenic amnesia. Different theories include:
- Freudian psychology states that psychogenic amnesia is an act of self-preservation, an alternative to suicide.
- Cognitive point-of-view states that this disorder utilizes the body’s personal semantic belief system to repress unwanted memories from entering the consciousness by altering neuropeptides and neurotransmitters released during stressful events, affecting the formation and recall of memory.
- “Betrayal trauma theory suggests that psychogenic amnesia is an adaptive response to childhood abuse. When a parent or other powerful figure violates a fundamental ethic of human relationships, victims may need to remain unaware of the trauma not to reduce suffering but rather to promote survival. Amnesia enables the child to maintain an attachment with a figure vital to survival, development, and thriving. Analysis of evolutionary pressures, mental modules, social cognitions, and developmental needs suggests that the degree to which the most fundamental human ethics are violated can influence the nature, form, and processes of trauma and responses to trauma.”
- Normal autobiographical memory processing is blocked by imbalance or altered release of stress hormones such as glucocorticoids and mineralocorticoids in the brain. The regions of expanded limbic system in the right hemisphere are more vulnerable to stress and trauma, affecting the body’s opioids, hormones, and neurotransmitters such as norepinephrine, serotonin, and neuropeptide Y. Increased levels of glucocorticoid and mineralocorticoid receptor density may affect the anterior temporal, orbitofrontal cortex, hippocampal, and amygdalar regions. These morphological changes may be caused by loss of regulation of gene expressions in those receptors along with inhibition of neurotrophic factors during chronic stress conditions.
- Stress may directly affect the medial temporal/diencephalic system, inhibiting the retrieval of autobiographical memories and producing a loss of personal identity. Negative feedback produced by this system may dampen the patient’s emotions, giving a perplexed or ‘flat’ appearance.
Treatments
Currently, various treatments are available for patients with psychogenic amnesia although no well-controlled studies on the effectiveness of different treatments exist.
- Psychoanalysis – uses dream analysis, interpretation and other psychoanalytic methods to retrieve memories; may also involve placing patients in threatening situations where they are overwhelmed with intense emotion.
- Medication and relaxation techniques – in conjunction with benzodiazepines and other hypnotic medications, the patient is urged to relax and attempt to recall memories. With the help of psychotherapy and learning their autobiographies from family members, most patients recover their memories completely.
It has been proposed that abreaction could be used in conjunction with midazolam to recover memories. This technique was used during the second World War but is currently much less popular. The technique is thought to work either through depressing the function of the cerebral cortex and therefore making the memory more tolerable when expressed, or through relieving the strength of an emotion attached to a memory which is so intense it suppresses memory function.
Some studies about psychogenic amnesia have concluded that psychotherapy is not connected to recovered memories of child sexual abuse. Data suggests that one’s amnesic recovered memory is spontaneous, and that this is triggered by abuse-related stimuli.
In popular culture
Memory loss due to emotional upset or shock has been recognized since at least the first century: Pliny the Elder wrote, “Nothing whatever, in man, is of so frail a nature as the memory; for it is affected by disease, by injuries, and even by fright; being sometimes partially lost, and at other times entirely so.”
Psychogenic amnesia is a common plot device in many films and books and other media. Examples include Shakespeare’s King Lear who experienced amnesia and madness following a betrayal by his daughters; the title character Nina in Nicolas Dalayrac’s opera of 1786 and the character of Jason Bourne as depicted in the Bourne film series; Jackie Chan in Who Am I?; the character Teri Bauer in 24; Goldie Hawn in Overboard; Leroy Jethro Gibbs in NCIS and the character Victoria Lord in One Life to Live.
Real life examples
- A man later identified as Edward Lighthart woke up in Seattle’s Discovery park, with supposed dissociative amnesia, on July 30, 2009, and briefly became a local mystery.
- A man discovered unconscious on August 31, 2004, in Richmond Hill, Georgia who adopted the pseudonym Benjaman Kyle.
Repressed memory
Repressed memory is a hypothetical concept used to describe a significant memory, usually of a traumatic nature, that has become unavailable for recall; also called motivated forgetting in which a subject blocks out painful or traumatic times in one’s life. This is not the same as amnesia, which is a term for any instance in which memories are either not stored in the first place (such as with traumatic head injuries when short term memory does not transfer to long term memory) or forgotten.
The term is used to describe memories that have been dissociated from awareness as well as those that have been repressed without dissociation. Repressed memory syndrome, the clinical term used to describe repressed memories, is often compared to psychogenic amnesia, and some sources compare the two as equivalent.
According to proponents of the hypothesis, repressed memories may sometimes be recovered years or decades after the event, most often spontaneously, triggered by a particular smell, taste, or other identifier related to the lost memory, or via suggestion during psychotherapy.
The existence of repressed memories is a controversial topic in psychology; some studies have concluded that it can occur in victims of trauma, while others dispute it. According to the American Psychological Association, it is not currently possible to distinguish a true repressed memory from a false one without corroborating evidence.
History
The concept was originated by Sigmund Freud in his 1896 essay Zur Ätiologie der Hysterie (“On the etiology of hysteria”). Freud abandoned his hypothesis between 1897 and 1905, replacing it during 1920–1923 with his impulse-based concept of Ego, super-ego, and id.
Research
Some research indicates that memories of child sexual abuse and other traumatic incidents may be forgotten. Evidence of the spontaneous recovery of traumatic memories has been shown, and recovered memories of traumatic childhood abuse have been corroborated.
Van der Kolk and Fisler’s research shows that traumatic memories are retrieved, at least at first, in the form of mental imprints that are dissociated. These imprints are of the affective and sensory elements of the traumatic experience. Clients have reported the slow emergence of a personal narrative that can be considered explicit (conscious) memory. The level of emotional significance of a memory correlates directly with the memory’s veracity. Studies of subjective reports of memory show that memories of highly significant events are unusually accurate and stable over time. The imprints of traumatic experiences appear to be qualitatively different from those of nontraumatic events. Traumatic memories may be coded differently than ordinary event memories, possibly because of alterations in attentional focusing or the fact that extreme emotional arousal interferes with the memory functions of the hippocampus.
Although research on repressed memory is limited, a few studies have suggested that memories of trauma that are forgotten and later recalled have a similar accuracy rate as trauma memories that had not been forgotten.
There has also been significant questioning of the reality of repressed memories. There is considerable evidence that rather than being pushed out of consciousness, the difficulty with traumatic memories for most people are their intrusiveness and inability to forget. One case that is held up as definitive proof of the reality of repressed memories, recorded by David Corwin has been criticized by Elizabeth Loftus and Melvin Guyer for ignoring the context of the original complaint and falsely presenting the sexual abuse as unequivocal and true when in reality there was no definitive proof.
Hypothesis
It has been speculated that repression may be one method used by individuals to cope with traumatic memories, by pushing them out of awareness (perhaps as an adaptation via psychogenic amnesia) to allow a child to maintain attachment to a person on whom they are dependent for survival. Researchers have proposed that repression can operate on a social level as well.
Controversy
The existence of repressed memory recovery has not been completely accepted by mainstream psychology, nor unequivocally proven to exist, and some experts in the field of human memory feel that no credible scientific support exists for the notions of repressed/recovered memories. One research report states that a distinction should be made between spontaneously recovered memories and memories recovered during suggestions in therapy.
Legal issues
Some criminal cases have been based on a witness’ testimony of recovered repressed memories, often of alleged childhood sexual abuse. In some jurisdictions, the statute of limitations for child abuse cases has been extended to accommodate the phenomena of repressed memories as well as other factors. The repressed memory concept came into wider public awareness in the 1980s and 1990s followed by a reduction of public attention after a series of scandals, lawsuits, and license revocations.
In a 1996 ruling, a US District Court allowed repressed memories entered into evidence in court cases. Jennifer Freyd writes that Ross Cheit’s case of suddenly remembered sexual abuse is one of the most well-documented cases available for the public to see. Cheit prevailed in two lawsuits, located five additional victims and tape-recorded a confession.
On 16 December 2005 the Irish Court of Criminal Appeal issued a certificate confirming a Misscarriage of Justice to a former nun Nora Wall whose 1999 conviction for child rape was partly based on Repressed Memory evidence. The judgement stated that: “There was no scientific evidence of any sort adduced to explain the phenomenon of ‘flashbacks’ and/or ‘retrieved memory’, nor was the applicant in any position to meet such a case in the absence of prior notification thereof.”
Recovered memory therapy
Recovered memory therapy (RMT) is a term coined by affiliates of the False Memory Syndrome Foundation referring to what they described as a range of psychotherapy methods based on recalling memories of abuse that had previously been forgotten by the patient. The term is not listed in DSM-IV or used by mainstream formal psychotherapy modality. Opponents of the therapy advance the hypothesis that therapy can create false memories through suggestion techniques; this hypothesis is controversial and has been neither proven nor disproven. Some research has shown evidence supporting the hypothesis, and this evidence is questioned by some researchers. It is possible for patients who retract their claims- after deciding their recovered memories are false- to suffer post-traumatic stress disorder due to the trauma of illusory memories. According to a book written in 1995, the number of reported retractions is small when compared to the large number of actual child sexual abuse cases.
Recovered memory therapy
Recovered memory therapy (RMT) is a term coined by affiliates of the False Memory Syndrome Foundation (FMSF) in the early 1990s, to refer what they described as a range of psychotherapy methods based on recalling memories of abuse that had previously been forgotten by the patient. It does not refer to a specific, recognized treatment method, but rather several controversial and/or unproven interviewing techniques, such as hypnosis and the use of sedative-hypnotic drugs. The term is not listed in DSM-IV or used by any mainstream formal psychotherapy modality.
Terminology
The term recovered memory therapy was coined between 1992 and 1993 by the False Memory Syndrome Foundation. The FMSF, an organization that advocates on behalf of individuals who claim they have been falsely accused of perpetrating child sexual abuse, hypothesized that RMT can result in patients recalling instances of sexual abuse from their childhood that may not have actually occurred. While not a therapeutic technique in and of itself, RMT generally is applied to such methods as hypnosis, age regression, drug-assisted interviewing (using substances such as sodium amytal), and guided visualization. It should be noted that while practiced by some individual therapists, these techniques were never recognized by the psychiatric or psychological community, and are generally not practiced in mainstream treatment modalities.
The term RMT has been called a reactionary construct used by activists affiliated with the False Memory Syndrome Foundation as a way to contest the efficacy of the trauma model of psychopathology. An inquiry into the practice by the Australian government found little support for or use of RMT from health professionals; rather the term was created by associations for political use. In October, 2007, Scientific American published an article critical of RMT. In a letter to the publication, the International Society for the Study of Trauma and Dissociation criticized the article for erroneously presenting the idea that there was a coherent method or training for something called ‘recovered memory therapy.’ Despite the lack of such a coherent method or training—the term sometimes crops up not only in the popular press but also in government inquiries, court proceedings, and position statements from psychologists’ professional associations.
Research
A range of studies have concluded that at least 10% of physical and sexual abuse victims forget the abuse. The rate of delayed recall of many forms of traumatic experiences (including natural disasters, kidnapping, torture and more) averages among studies at approximately 15%, with the highest rates resulting from child sexual abuse, military combat, and witnessing a family member murdered. The rate of recall of previously forgotten traumatic events was shown by Elliot and Briere (1996) to be unaffected by whether or not the victim had a history of being in psychotherapy. Williams found that among women with confirmed histories of sexual abuse, approximately 38% did not recall the abuse 17 years later, especially when it was perpetrated by a someone familiar to them. Hopper cites several studies of corroborated abuse in which some abuse victims will have intervals of complete or partial amnesia for their abuse. Peer reviewed and clinical studies have documented the existence of recovered memory, one list cites 43 legal cases where an individual whose claim to have recovered a repressed memory has been accepted by a court.
A 1996 interview survey of 711 women reported that forgetting and later remembering childhood sexual abuse is not uncommon; more than a quarter of the respondents who reported abuse also reported forgetting the abuse for some period of time and then recalling it on their own. Of those who reported abuse, less than 2% reported that the recall of the abuse was assisted by a therapist or other professional.
A review article on potentially harmful therapies listed RMT as a treatment that will probably produce harm in some who receive it. Richard Ofshe, a member of the advisory board to the FMSF, describes the practice of “recovering” memories as fraudulent and dangerous.
Studies by Elizabeth Loftus and others have concluded that it is possible to produce false memories of childhood incidents. The experiments involved manipulating subjects into believing that they had some fictitious experience in childhood, such as being lost in a shopping mall at age 6. This involved using a suggestive technique called “familial informant false narrative procedure,” in which the experimenter claims the validity of the false event is supported by a family member of the subject. The study has been used to support the theory that false memories of traumatic sexual abuse can be implanted in a patient by therapists. However, the techniques used in these studies do not resemble any approved or mainstream treatment modality, and there are criticisms that the implanted events used are not emotionally comparable to sexual abuse. Further, the false memories were successfully created only 30% of the time across multiple studies. Critics contend that Loftus’s conclusions overreach the evidence.
Some patients later retract memories they had previously believed to be recovered. Whilst false or contrived memories are possible reasons for such retractions, other explanations suggested for the retraction of allegations of abuse made by children and adults include guilt, a feeling of obligation to protect their family and a reaction to familial stress rather than a genuine belief that their memories are false. The number of retractions is reported to be small compared to the actual number of child sexual abuse allegations made based on recovered memories.
A study at the Dissociative Disorders and Trauma Program of the McLean Hospital concluded that that recovered memories are mostly unconnected to psychotherapeutic treatment and that memories are often corroborated by independent evidence, often appearing while home or with family and friends, with suggestion being generally denied as a factor in recovering memories. Very few participants were in therapy during their first memory recovery and a majority of participants in this study found strong corroboration of their recovered memories.
Professional guidelines
There are several individuals and groups that have published guidelines, criticisms or cautions about recovered memory therapy and techniques to stimulate recall:
- In the Brandon Report, a set of training, practice, research and professional development recommendations, the United Kingdom’s Royal College of Psychiatrists advised psychiatrists to avoid use of RMT or any “memory recovery techniques”, citing a lack of evidence to support the accuracy of memories recovered in this way.
- In 2004, the government of the Health Council of the Netherlands issued a report in response to inquiries from professionals regarding RMT and memories of traumatic child sexual abuse. The Health Council stated that while traumatic childhood experiences were major risk factors for psychological problems in adulthood, most traumatic memories are well remembered but can be forgotten or become inaccessible though the influence of specific circumstances precludes a simple description of the relationship between memory and trauma. The report also notes that memories can be confabulated, re-interpreted and even apparently vivid or dramatic memories can be false, a risk that is increased when therapists use suggestive techniques, attempt to link symptoms to past trauma, with certain patients and through the use of methods to stimulate memories.
- The Australian Hypnotherapists Association (AHA) issued a similar statement, for contexts where false memories of child sexual abuse may arise. The AHA acknowledges that child sexual abuse is serious, damaging and at least some memories are genuine, while cautioning that some questioning techniques and interventions may lead to illusory memories leading to false beliefs about abuse.
- The Canadian Psychological Association has issued guidelines for psychologists addressing recovered memories. Psychologists are urged to be aware of their limitations in knowledge and training regarding memory, trauma and development and “that there is no constellation of symptoms which is diagnostic of child sexual abuse”. The guidelines also urge caution and awareness of the benefits and limitations of “relaxation, hypnosis, guided imagery, free associations, inner child exercises, age regression, body memory interpretation, body massage, dream interpretation, and the use of projective techniques” and special caution regarding any legal involvement of memories, abuse and therapy.
Legal issues
Discussing RMT in parliament in 1995, an Australian state Minister for Health, Dr Andrew Refshauge – a former medical practitioner – stated that the general issue of admissibility of evidence based on recovered memories was one for the Attorney General. In 2004 Australian Counseling Association issued a draft position statement regarding recovered memories in which they informed their membership of possible legal difficulties if they affirm accusations as true based solely upon discussion of a patient’s recovered memories without adequate corroborating evidence.
A degree of controversy does remain within legal circles, with some holding the view that therapists and courts should consider repressed memories the same as they consider regular memories. Three relevant studies state that repressed memories are “no more and no less accurate than continuous memories.”
Recovered memory therapy was an issue in the criminal trials of some Catholic priests accused of fondling or sexually assaulting juvenile-turned-adult parishioners.
Several court cases awarded multi-million dollar verdicts against Minnesota psychiatrist Diane Bay Humenansky, who used hypnosis and other suggestive techniques associated with RMT, resulting in accusations by several patients against family members, that were later found to be false.
In the UK, a woman who said she had falsely accused her father of rape successfully sued the hospital and psychologist who had treated her with what she described as a form of RMT and was awarded a large out-of-court settlement.
Fugue state
A fugue state, formally dissociative fugue or psychogenic fugue (DSM-IV Dissociative Disorders 300.13), is a rare psychiatric disorder characterized by reversible amnesia for personal identity, including the memories, personality and other identifying characteristics of individuality. The state is usually short-lived (hours to days), but can last months or longer. Dissociative fugue usually involves unplanned travel or wandering, and is sometimes accompanied by the establishment of a new identity. After recovery from fugue, previous memories usually return intact, but there is complete amnesia for the fugue episode. Additionally, an episode is not characterized as a fugue if it can be related to the ingestion of psychotropic substances, to physical trauma, to a general medical condition, or to psychiatric conditions such as delirium, dementia, bipolar disorder or depression. Fugues are usually precipitated by a stressful episode, and upon recovery there may be amnesia for the original stressor (Dissociative Amnesia).
Clinical definition
The etiology of the fugue state is related to Dissociative Amnesia, (DSM-IV Codes 300.12) which has several other subtypes: Selective Amnesia, Generalised Amnesia, Continuous Amnesia, Systematised Amnesia, in addition to the subtype Dissociative Fugue.
Unlike retrograde amnesia (which is popularly referred to simply as “amnesia”, the state where someone forgets events before brain damage), Dissociative Amnesia is not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication, DSM-IV Codes 291.1 & 292.83) or a neurological or other general medical condition (e.g., Amnestic Disorder due to a head trauma, DSM-IV Codes 294.0). It is a complex neuropsychological process.
As the person experiencing a Dissociative Fugue may have recently suffered the reappearance of an event or person representing an earlier life trauma, the emergence of an armoring or defensive personality seems to be for some, a logical apprehension of the situation.
Therefore, the terminology fugue state may carry a slight linguistic distinction from Dissociative Fugue, the former implying a greater degree of motion. For the purposes of this article then, a fugue state would occur while one is acting out a Dissociative Fugue.
The DSM-IV defines as:
- sudden, unexpected travel away from home or one’s customary place of work, with inability to recall one’s past,
- confusion about personal identity, or the assumption of a new identity, or
significant distress or impairment.
The Merck Manual defines Dissociative Fugue as:
- One or more episodes of amnesia in which the inability to recall some or all of one’s past and either the loss of one’s identity or the formation of a new identity occur with sudden, unexpected, purposeful travel away from home.
- In support of this definition, the Merck Manual further defines Dissociative Amnesia as:
- An inability to recall important personal information, usually of a traumatic or stressful nature, that is too extensive to be explained by normal forgetfulness.
Diagnosis
A doctor may suspect dissociative fugue when people seem confused about their identity or are puzzled about their past or when confrontations challenge their new identity or absence of one. The doctor carefully reviews symptoms and does a physical examination to exclude physical disorders that may contribute to or cause memory loss. A psychologic examination is also done. Sometimes dissociative fugue cannot be diagnosed until people abruptly return to their pre-fugue identity and are distressed to find themselves in unfamiliar circumstances. The diagnosis is usually made retroactively when a doctor reviews the history and collects information that documents the circumstances before people left home, the travel itself, and the establishment of an alternative life.
Case studies
- Agatha Christie disappeared on 3 December 1926 only to reappear eleven days later in a hotel in Harrogate, apparently with no memory of the events which happened during that time span.
- Shirley Ardell Mason also known as “Sybil” would disappear and then reappear with no recollection of what happened during the time span. She recalls “being here and then not here” and having no identity of herself; it should be noted that she also suffered from what was formerly called “Multiple Personality Disorder”.
- Jody Roberts, a reporter for the Tacoma News Tribune, went missing in 1985, only to be found 12 years later in Sitka, Alaska, living under the name of “Jane Dee Williams.” While there were some initial suspicions that she had been faking amnesia, some experts have come to believe that she genuinely suffered a protracted fugue state.
- David Fitzpatrick, a sufferer of dissociative fugue disorder, from the United Kingdom, was profiled on Channel Five’s television series Extraordinary People. He entered a fugue state on December 22, 2005, and is still working on regaining his entire life’s memories.
- Hannah Upp, a teacher from New York, went missing on August 28, 2008. She was rescued from the New York Harbor on September 16 with no recollection of the time in between. The episode was diagnosed as dissociative fugue.
Pop culture references
- In the television show Breaking Bad the main character fakes a fugue state to cover up his other activities.
- During the Doctor Who episode The Next Doctor it is discovered by the Tenth Doctor that the future incarnation of himself is actually a man named Jackson Lake, suffering a fugue state after the loss of his family to the Cybermen.
- In the series Twin Peaks, a girl named Ronette Pulaski is found walking down train tracks in a fugue state (though the term is not actually used).
- David Lynch has said that the character of Fred Madison in his 1997 film Lost Highway is in a fugue state.
- In the Buffy the Vampire Slayer (TV series) episode Bring on the Night (Buffy the Vampire Slayer) (season 7 episode 10), Dawn says in reference to Andrew, “Or maybe he’s in a fugue state?”
- The character Eddie Morra in the 2011 film Limitless experiences fugue states whilst on the fictional drug NZT.
- The film Nurse Betty is about a Kansas City waitress (played by Renee Zellweger) who goes into a fugue state after seeing her husband scalped.
- In the Film and Novel Primal Fear the supporting character Aaron Stampler appears to slip frequently in to and out of a fugue state but it is later revealed to be an act.
- In the Australian television series Neighbours a main character Harold Bishop went AWOL for five years in a putative fugue state.
Lacunar amnesia
Lacunar amnesia is the loss of memory about one specific event. It is a type of amnesia that leaves a lacuna (a gap) in the record of memory. According to Steven Johnson, (the author of Mind Wide Open: Your Brain and the Neuroscience of Everyday Life):
“Scientists believe memories are captured and stored by two separate parts of the brain, the hippocampus, the normal seat of memory, and the amygdala, one of the brain’s emotional centers. People who, due to hippocampus damage, are incapable of forming long-term memories can still form subconscious memories of traumatic events if their amygdala is intact. Someone suffering from the Memento condition would likely have a feeling of general unease encountering a person who had harmed them in the past, though they wouldn’t be able to put their finger on why. As the plot of Eternal Sunshine correctly suggests, the brain is designed to preserve emotionally strong memories. Even amnesiacs, under the right circumstances, can remember their past feelings.”
Furthermore, according to Alex Chadwick speaking on NPR:
“Some scientists now believe that memories effectively get rewritten every time they’re activated. Studies on rats suggest that if you block a crucial chemical process during the execution of a learned behavior – pushing a lever to get food, for instance – the learned behavior disappears. The rat stops remembering. Theoretically, if you could block that chemical reaction in a human brain while triggering a specific memory, you could make a targeted erasure. Think of a dreadful fight with your girlfriend while blocking that chemical reaction, and zap! The memory’s gone.”
Daniel Goleman, in his book Vital Lies, Simple Truths, defines a lacuna as :
“… lacuna, from the Latin for gap or hole, to refer to the sort of mental apparatus that diversionary schemas represent. A lacuna is, then, the attentional mechanism that creates a defensive gap in awareness. Lacunas, in short, create blind spots “
Popular culture
This type of amnesia is used as a plot element in the movie Eternal Sunshine of the Spotless Mind, in which a company (appropriately named Lacuna) offers the service of having a specific person erased from someone’s memories by removing all memories of them.
Similarly, in the manga Fruits Basket, the character Hatori Sohma has the ability to erase a persons memories. This ability is utilised by the head of the family, Akito, who instructed Hatori to use it when people outside the family discovered their secret. He also had to use the ability to make his fiance, Kana, forget about him because he’d caused her too much pain.
Childhood amnesia
Childhood amnesia, also known as infantile amnesia, is the common inability of adults to remember the earliest years of their childhood.
Characterization and background
Infantile, or childhood amnesia is characterized by the relative absence of memory before 4 years of age. It is not the complete absence of memories, but the relative scarcity of memories from infancy —a scarcity that cannot be accounted for by a forgetting curve. Additionally, the boundary is malleable and can be influenced by both individual experiences and cultural factors.
Research has demonstrated that children are adept learners and are quick to acquire and retain information. Children do remember events; however, these memories accessible as children are lost to infantile amnesia in adulthood.
Research on childhood amnesia generally uses easily-verifiable, highly salient events such as the birth of a sibling to test recall to avoid difficulties with unreliability of reporting and memories of children in general.
Early observations
Childhood amnesia, despite being a universal human experience, was only first formally studied in 1893 by the psychologist Caroline Miles in her article “A study of individual psychology”, published in the American Journal of Psychology. In 1904 G. Stanley Hall noted the phenomenon in his book Adolescence, but it was Sigmund Freud who offered one of the first, most famous, and most controversial descriptions and explanations of childhood amnesia when he tied the phenomenon in with psychoanalysis.
Modern observations
It has been suggested that the average age of the first memories is three years, six months, with the vast majority of subjects dating their first recollection somewhere between ages two and five years. Early (i.e. childhood) and late (i.e. adult) memories show few differences in emotional versus factual, and episodic versus non-episodic content of the memories. Very few memories of adults precede 30 months, and those that are reported at this time show considerable confabulation with individuals unable to tell the difference between a memory of an event and simple knowledge of the event (i.e. gained from discussion by others).
Proposed explanations
Since Miles first officially documented childhood amnesia as a psychological phenomenon, many theories of its causes and character have been developed and none have proven significantly more useful or true than any others.
Freud’s trauma explanation
Sigmund Freud’s theories of psychosexual development are highly intertwined with childhood experiences. In what is now published as The Standard Edition of the Complete Psychological Works of Sigmund Freud, Freud theorized that childhood amnesia is the result of the mind’s attempt to repress memories of traumatic events that, according to Freud, necessarily occur in the psychosexual development of every child. This would lead to the repression of the majority of the memories of the first years of life. Freudian theory, including his explanation for childhood amnesia, has been criticized for extensive use of anecdotal evidence rather than scientific research, and said to frequently permit multiple interpretations.
Physical development explanation
Childhood amnesia may also be due to the lack of neurological development of the infant brain, preventing the creation of long term or autobiographical memories. Two key structures in the neuroanatomy of memory, the hippocampus and prefrontal cortex, do not develop into mature structures until the age of three or four years. These structures are known to be associated with the formation of autobiographical memories of the type notably missing from adult recollection of early childhood.
Language explanation
The incomplete development of language in young children may be a cause of childhood amnesia in that infants do not have the language capacity to encode autobiographical memories in a manner that their language-based adult selves can interpret correctly. The typical schedule of language development seems to support this theory. Babies of one year old tend to be limited to one word utterances, and childhood amnesia predicts that adults have very few, if any, memories of this time. By the age of three, children are capable of two or three word phrases, and by age five their speech already resembles adult speech. This language development seems to very much correspond to childhood amnesia because it is around the age of three to four that is the time of most adults’ earliest recallable memory. Pre-verbal children shown a picture of a memorable event from a year previously demonstrate verbal and nonverbal recall, but describe the experience solely using language skills available at the time the memory was created.
Emotion explanation
The amygdala-governed memory pathway (which is primarily concerned with emotions and emotional content of memories) and hippocampus-governed pathway (which concerns primarily autobiographical memories) are generally independent, but emotions and the amygdala are known to play a role in the encoding of memories typically associated with the hippocampus. It has been suggested that the differences between the emotions experienced by infants and adults may be a cause of childhood amnesia. The idea that highly emotional events can stimulate and improve recall (the “flashbulb memory”) is still being debated and belief in these types of memories is the primary proof of the effects of emotion on memory.
Context explanation
The difference in perspective that children and adults experience of the world may be a cause of childhood amnesia. For children, their physical perception of objects and their understanding of people and events are very different from the world of the adult. Moreover, an infant’s basic understanding of the universe, like object permanence or occlusion effects, is not innate at birth. This leads to a disparity in retrieval cues used by the adult and those used by the infant, who will encode memories without many of these principles that are ingrained in the mind of the adult trying to recollect. This different context could lead to the inability of the adult to remember his earliest years at all. An infant’s development of a theory of mind is linked to the ability to form an episodic memory, and the development of the ability to contextualize memories at the age of 3 to 5 may be the source of people’s first retrievable memories. The development of self-awareness at around two years of age has also been proposed as an explanation, where memories are inherently associated with one’s sense of self, such that memories encoded before self-awareness develops are not comprehensible to the individual even though some information is stored in the brain.
Patterns of childhood amnesia
Much recent research has found patterns in the extent of childhood amnesia. The most prominent patterns are gender and race.
Males versus females
In general the earliest recollections of females are earlier and more vivid than those of males. It has been suggested that this pattern is due to differences in how males and females interact as children, especially the types of conversations they have.
Race and ethnicity
Race has also been shown to play a role in the effect of childhood amnesia. One study found that Europeans had later first retrievable memories than Māori, and Asians had still later ones. It has been suggested that the importance of the past in Māori culture may have something to do with their particularly early first retrievable memory.
Transient global amnesia
Transient global amnesia (TGA) is “one of the most striking syndromes in clinical neurology” whose key defining characteristic is temporary but almost total disruption of short-term memory with a range of problems accessing older memories. A person in a state of TGA exhibits no other signs of impaired cognitive functioning but recalls only the last few moments of consciousness plus deeply-encoded facts of the individual’s past, such as his or her own name.
Symptoms
A person having an attack of TGA has almost no capacity to establish new memories, but generally appears otherwise mentally alert and lucid, possessing full knowledge of self-identity and identity of close family, and maintaining intact perceptual skills and a wide repertoire of complex learned behavior. The individual simply cannot recall anything that happened outside the last few minutes, while memory for more temporally distant events may or may not be largely intact. The degree of amnesia is profound, and, in the interval during which the individual is aware of his or her condition, is often accompanied by anxiety. The diagnostic criteria for TGA, as defined for purposes of clinical research, include:
- The attack was witnessed by a capable observer and reported as being a definite loss of recent memory (anterograde amnesia).
- There was an absence of clouding of consciousness or other cognitive impairment other than amnesia.
- There were no focal neurological signs or deficits during or after the attack.
- There were no features of epilepsy, or active epilepsy in the past two years, and the patient did not have any recent head injury.
- The attack resolved within 24 hours.
Progression of a TGA event
This onset of TGA is generally fairly rapid, and its duration varies but generally lasts between 2 to 8 hours. A person experiencing TGA typically has memory only of the past few minutes or less, and cannot retain new information beyond that period of time. One of its bizarre features is perseverance, in which the victim of an attack faithfully and methodically repeats statements or questions, complete with profoundly identical intonation and gestures “as if a fragment of a sound track is being repeatedly rerun.” This is found in almost all TGA attacks and is sometimes considered a defining characteristic of the condition. The individual experiencing TGA retains social skills and older significant memories, almost always including knowing his or her own identity and the identity of family members, and the ability to perform various complex learned tasks including driving and other learned behavior; one individual “was able to continue putting together the alternator of his car.” Though outwardly appearing normal, a person in TGA is disoriented in time and space, perhaps knowing neither the year nor where he or she resides. Although confusion is sometimes reported, others consider this an imprecise observation, but an elevated emotional state (compared to patients experiencing Transient Ischemic Attack, or TIA) is common. In a large survey, 11% of individuals in a TGA state were described as exhibiting “emotionalism” and 14% “fear of dying”. The attack lessens over a period of hours, with older memories returning first, and the repetitive fugue slowly lengthening so that the victim retains short-term memory for longer periods. While seemingly back to normal within 24 hours, there are subtle effects on memory that can persist longer. In the majority of cases there are no long-term effects other than a complete lack of recall for this period of the attack and an hour or two before its onset. There is emerging evidence for observable impairments in a minority of cases weeks or even years following a TGA attack.
There is also evidence that the victim is aware that something is not quite right, even though they can’t pinpoint it. The person suffering from the attack may vocalize signs that ‘they just lost their memory’, or that they believed they had a stroke, although they aren’t aware of the other signs that they are displaying. The main sign of this condition is the repetitive actions of something that is not usually repeated.
Differential diagnosis
A differential diagnosis should include:
- Thrombosis of the basilar artery
- Cardioembolic stroke
- Complex partial seizures
- Frontal lobe epilepsy
- Lacunar syndromes
- Migraine variants
- Posterior cerebral artery stroke
- Syncope and related paroxysmal spells
- Temporal lobe epilepsy
- If the event lasts less than one hour, transient epileptic amnesia (TEA) might be implicated.
- If the condition lasts longer than 24 hours, it is not considered TGA by definition. A diagnostic investigation would then probably focus on some form of undetected ischemic attack or cranial bleed.
Causes
The underlying cause of TGA remains enigmatic. The leading hypotheses are some form of epileptic event, a problem with blood circulation around, to or from the brain, or some kind of migraine-like phenomenon. The differences are sufficiently meaningful that transient amnesia may be considered a heterogeneous clinical syndrome with multiple etiologies, corresponding mechanisms, and differing prognoses.
Precipitating events
TGA attacks are associated with some form of precipitating event in at least one-third of cases. In females, this event is more often of a strong emotional character; in males, it is more often related to some physical exertion. The most commonly cited precipitating events include vigorous exercise (including sexual intercourse), swimming in cold water or enduring other temperature changes, and emotionally traumatic or stressful events. There are reports of TGA-like conditions following certain medical procedures and disease states. There is a slight (2%) familial incidence.
If the definition of a precipitating event is widened to include events days or weeks earlier, and to take in emotionally stressful burdens such as money worries, attending a funeral or exhaustion due to overwork or unusual childcare responsibilities, a large majority, over 80%, of TGA attacks are said to correlate with precipitating events.
The role of psychological co-factors has been addressed by some research. It is the case that people in a state of TGA exhibit measurably elevated levels of anxiety and/or depression. Emotional instability may leave some people vulnerable to stressful triggers and thus be associated with TGA. Individuals who have experienced TGA, compared with similar people with TIA, are more likely to have some kind of emotional problem (such as depression or phobias) in their personal or family history or to have experienced some kind of phobic or emotionally challenging precipitating event.
Vascular hypotheses
Cerebral ischemia is a frequently-disputed possible cause, at least for some segment of the TGA population, and until the 1990s it was generally thought that TGA was a variant of transient ischemic attack (TIA) secondary to some form of cerebrovascular disease. Those who argue against a vascular cause point to evidence that those experiencing TGA no more likely than the general population to have subsequent cerebral vascular disease. In fact, “in comparison with TIA patients, TGA patients had a significantly lower risk of combined stroke, myocardial infarct, and death.”
Other vascular origins remain a possibility, however, according to research of jugular vein valve insufficiency in patients with TGA. In these cases, mostly men, TGA has followed vigorous exertion. One current hypothesis is that TGA may be due to venous congestion of the brain, leading to ischemia of structures involved with memory, such as the hippocampus. It has been shown that performing a Valsalva maneuver (involving “”bearing down”” and increasing breath pressure against a closed glottis, which occurs frequently during exertion) may be related to retrograde flow of blood in the jugular vein, and therefore, presumably, cerebral blood circulation, in patients with TGA.
Migraine
A history of migraine is a statistically significant risk factor identified in the medical literature. “When comparing TGA patients with normal control subjects… the only factor significantly associated with an increased risk for TGA was migraine.” 14% of people with TGA had a history of migraine in one study, and approximately a third of the participants in another clinical study reported such a history.
However, migraine does not appear to occur simultaneously with TGA nor serve as a precipitating event. Headache frequently occurs during TGA, as does nausea, both symptoms often associated with migraine, but it appears that these do not indicate migraine in patients during a TGA event. The connection remains conceptual, and muddied further by a lack of consensus about the definition of migraine itself, and by the differences in age, gender, and psychological characteristics of migraine sufferers when compared to those variables in the TGA cohort.
Epilepsy
Amnesia is often a symptom in epilepsy, and for that reason people with known epilepsy are disqualified from most studies of TGA. In a study where strict criteria were applied to TGA diagnosis, no epileptic features were seen in EEGs of over 100 patients with TGA. However, despite the fact that EEG readings are usually normal during a TGA attack, and other usual symptoms of epilepsy are not observed with TGA it has been speculated that some initial epileptic attacks present as TGA. The observation that 7% of people who experience TGA will develop epilepsy calls into question whether those case are, in fact, TGA or transient epileptic amnesia (TEA). TEA attacks tend to be short (under one hour) and tend to recur, so that a person who has experienced both repeated attacks of temporary amnesia resembling TGA and if those events lasted less than one hour is very likely to develop epilepsy.
There is additional speculation that atypical cases of TEA in the form of nonconvulsive status epilepticus may present with duration similar to TGA. This may constitute a distinct subgroup of TGA. TEA, as opposed to “pure” TGA, is also characterized by “two unusual forms of memory deficit …: (i) accelerated long-term forgetting (ALF): the excessively rapid loss of newly acquired memories over a period of days or weeks and (ii) remote autobiographical memory loss: a loss of memories for salient, personally experienced events of the past few decades.”
Whether an amnestic event is TGA or TEA thus presents a diagnostic challenge, especially in light of the recently-published descriptions of possible long-term cognitive deficits with (presumably correctly-diagnosed) TGA.
Other putative associations
There have been assertions of a possible link between TGA and the use of statins (a class of drug used in treating cholesterol).
Prognosis
The prognosis of “pure” TGA is very good. It does not affect mortality or morbidity and unlike earlier understanding of the condition, TGA is not a risk factor for stroke or ischemic disease. Rates of recurrence are variously reported, with one systematic calculation suggesting the rate is under 6% per year. TGA “is universally felt to be a benign condition which requires no further treatment other than reassurance to the patient and their family.” “The most important part of management after diagnosis is looking after the psychological needs of the patient and his or her relatives. Seeing a once competent and healthy partner, sibling or parent become incapable of remembering what was said only a minute ago is very distressing, and hence it is often the relatives who will require reassurance.”
TGA may have multiple etiologies and prognoses. Atypical presentations may masquerade as epilepsy and be more properly considered TEA. In addition to such probable TEA cases, some people experiencing amnestic events diverging from the diagnostic criteria articulated above may have a less benign prognosis than those with “pure” TGA.
Recently, moreover, both imaging and neurocognitive testing studies question whether TGA is as benign as has been thought. MRI scans of the brain in one study showed that among people who had experienced TGA, all had cavities in the hippocampus, and these cavities were far more numerous, larger, and more suggestive of pathological damage than in either healthy controls or a large control group of people with tumor or stroke. Verbal and cognitive impairments have been observed days after TGA attacks, of such severity that the researchers estimated the effects would be unlikely to resolve within a short time frame. A large neurocognitive study of patients more than a year after their attacks have shown persistent effects consistent with amnestic mild cognitive impairment (MCI-a) in a third of the people who had experienced TGA. In another study, “selective cognitive dysfunctions after the clinical recovery” were observed, suggesting a prefrontal impairment. These dysfunctions may not be in memory per se but in retrieval, in which speed of access is part of the problem among people who have had TGA and experience ongoing memory problems.
Epidemiology
The estimated annual incidence of TGA varies from a minimum of 2.9 cases per 100,000 population (in Spain) and 5.2 per 100,000 (in USA), but among people aged over 50, the rate of TGA incidence is reported to range from approximately 23 per 100,000 (in a US population) to 32 per 100,000 (in a population in Scandinavia).
TGA is most common in people between age 56 and 75, with the average age of a person experiencing TGA being approximately 62.
Source amnesia
Source amnesia is an explicit memory disorder in which someone can recall certain information, but not where or how it was obtained.
Process and experimentation
The disorder is particularly episodic, where source or contextual information surrounding facts are severely distorted or unable to be recalled. Via the use of the Wisconsin Card Sorting Task (WCST) developed by Esta Berg in 1948, Positron Emission Tomography (PET), and explicit and implicit memory tests, researchers have performed extensive empirical research on source-amnesiacs and concluded or suggested neuropsychological genesis.
Daniel Schacter and Endel Tulving have each proposed that memory for facts is differentiated from memory for context. The neuropsychological implications as in brain maturation, deterioration in the normal aging course, and damage are conveyed. The organic deterioration of the frontal lobes in the process of normal aging has a greater influence on episodic memory than perhaps premature lobes in young children. Source amnesia has the ability to alter one’s confidence in their memory encoded in differing conditions (e.g., while conscious or in dreaming), as in memory distrust syndrome, an inclusive disorder. Source amnesia was first presented and examined in the hypnotic environment, and further understanding the human memory process is essential in unraveling this condition.
Phenomena
As source amnesia prohibits recollection of the context specific information surrounding facts in experienced events, there is also the inclusive case of confusion concerning the content or context of events, a highly attributable factor to confabulation in brain disease. Such confusion was termed memory distrust syndrome by Gudjonsson and MacKeith. A condition similar to source amnesia sometimes occurs in dreams, when the dreamer has some knowledge about details of the imaginary environment but has no idea how they learned this information.
Source amnesia has been theorized to partially account (in some cases alongside confirmation bias) for particularly persistent, common misconceptions. Unable to place a known “fact” into the context of an unreliable source, some individuals may subconsciously re-assign the information an ambiguous or more trustworthy origin.
Memory distrust syndrome
Memory distrust syndrome is a term coined by Gísli Guðjónsson and James MacKeith in 1982, to describe those who distrust their own memories and are motivated to rely on external (non-self) sources to verify the accuracy of memories.
Memory distrust syndrome is associated with source amnesia, which prohibits full recollection of how one acquired a specific memory. Additionally, memory distrust syndrome involves confusion concerning the content or context of events, a highly attributable factor to confabulation in brain disease.
The overwhelming propensity to accept information from external sources (i.e. an interrogator) based on the influence of susceptibility has led to well documented false confessions. In addition, the credibility of a witness account who suffers from memory distrust syndrome is more questionable. In a parallel situation, amnesic individuals may have a greater propensity to have their memory manipulated and perhaps perform non-advantageous acts on the “direction” of external sources and have difficulty in differentiating imaginary and real experiences. Since the criminal law system considers source amnesia pathology to be an identified and natural occurrence, psychiatrists should increasingly take assessment and identification measures to isolate such a disorder in accused individuals and eye-witnesses.
Blackout (alcohol-related amnesia)
A blackout is a phenomenon caused by the intake of alcohol or other substance in which long term memory creation is impaired or there is a complete inability to recall the past. Blackouts are frequently described as having effects similar to that of anterograde amnesia, in which the subject cannot create memories after the event that caused amnesia. ‘Blacking out’ is not to be confused with the mutually exclusive act of ‘passing out’, which means loss of consciousness. Research on alcohol blackouts was begun by E. M. Jellinek in the 1940s. Using data from a survey of Alcoholics Anonymous (AA) members, he came to believe that blackouts would be a good predictor of alcoholism. However, there are conflicting views as to whether this is true.
Alcohol and long-term memory
Various studies have also proven links between general alcohol consumption and its effects on memory creation. Particularly, these studies have shown that associations made between words and objects when intoxicated are less easily recalled than associations made when not intoxicated. Later blackout-specific studies have indicated that alcohol specifically impairs the brain’s ability to take short-term memories and experiences and transfer them to long-term memory.
It is a common misconception that blackouts generally occur only to alcoholics; research suggests that binge drinkers, such as college students, are often at risk as well. In a 2002 survey of college students by researchers at Duke University Medical Center, 40% of those surveyed who had consumed alcohol recently reported having experienced a blackout within the preceding year.
Types of blackouts
Blackouts can generally be divided into two categories, “en bloc” blackouts, and “fragmentary” blackouts. En bloc blackouts are classified by the inability to later recall any memories from the intoxicated period, even when prompted. These blackouts are characterized also by the ability to easily recall things that have occurred within the last 2 minutes, yet inability to recall anything prior to this period. As such, a person experiencing an en bloc blackout may not appear to be doing so, as they can carry on conversations or even manage to accomplish difficult feats. It is difficult to determine the end of this type of blackout as sleep typically occurs before they end. Fragmentary blackouts are characterized by the ability to recall certain events from an intoxicated period, yet be unaware that other memories are missing until reminded of the existence of these ‘gaps’ in memory. This phenomenon is also termed a brownout. Research indicates that fragmentary blackouts, or brownouts are far more common than en bloc blackouts.
Causes
Blackouts are commonly associated with the consumption of large amounts of alcohol; however, surveys of drinkers experiencing blackouts have indicated that they are not directly related to the amount of alcohol consumed. Respondents reported they frequently recalled having “drunk as much or more without memory loss”, compared to instances of blacking out. Subsequent research has indicated that blackouts are most likely caused by a rapid increase in a person’s blood-alcohol concentration. One study, in particular, resulted in subjects being stratified easily into two groups, those who consumed alcohol very quickly, and blacked out, and those who did not black out by drinking alcohol slowly, despite being extremely intoxicated by the end of the study.
Other GABA-A Agonist Drugs
Benzodiazepines such as clonazepam (Klonopin), diazepam (Valium), and alprazolam (Xanax), and Barbiturates, such as Phenobarbital which also act as GABA-A agonists, are known to cause blackouts as a result of high dose use.
Predisposition to blackouts
Research indicates that some users of alcohol, particularly those with a history of blackouts, are predisposed to experience blackouts more frequently than others. One such study indicated a link between prenatal exposure to alcohol and vulnerability towards blackouts, in addition to the oft-cited link between this type of exposure and alcoholism. Alternatively, another study has indicated that there appears to be a genetic predisposition towards blacking out, suggesting that some individuals are made to be susceptible to alcohol related amnesia.
Korsakoff’s syndrome
Korsakoff’s syndrome (also called Korsakov’s syndrome, Korsakoff’s psychosis, or amnesic-confabulatory syndrome), is a neurological disorder caused by the lack of thiamine (vitamin B1) in the brain. The syndrome is named after Sergei Korsakoff, the neuropsychiatrist who popularized the theory.
Symptoms
There are six major symptoms of Korsakoff’s syndrome:
- anterograde amnesia
- retrograde amnesia, severe memory loss
- confabulation, that is, invented memories which are then taken as true due to gaps in memory sometimes associated with blackouts
- meager content in conversation
- lack of insight
- apathy – the patients lose interest in things quickly and generally appear indifferent to change.
These symptoms are caused by a deficiency of thiamine (vitamin B1), which is thought to cause damage to the medial thalamus and possibly to the mammillary bodies of the hypothalamus as well as generalized cerebral atrophy.
When Wernicke’s encephalopathy accompanies Korsakoff’s syndrome, the combination is called the Wernicke-Korsakoff syndrome. Korsakoff’s is a continuum of Wernicke’s encephalopathy, though a recognised episode of Wernicke’s is not always obvious.
Korsakoff’s involves neuronal loss, that is, damage to neurons; gliosis which is a result of damage to supporting cells of the central nervous system; and hemorrhage or bleeding in mammillary bodies. Damage to the dorsomedial nucleus or anterior group of the thalamus (limbic-specific nuclei) is also associated with this disorder.
Signs
- Apathy
- Ataxia
- Coma
- Confabulation
- Paralysis of muscles controlling the eye
- Retrograde and anterograde amnesia
- Tremor
- Anosognosia – Lack of insight to or awareness of the condition
Treatment
It was once assumed that anyone suffering from Korsakoff’s syndrome would eventually need full time care. This is still often the case, but rehabilitation can help regain some, often limited, level of independence. Treatment involves the replacement or supplementation of thiamine by intravenous (IV) or intramuscular (IM) injection, together with proper nutrition and hydration. However, the amnesia and brain damage caused by the disease does not always respond to thiamine replacement therapy. In some cases, drug therapy is recommended. If treatment is successful, improvement will become apparent within two years although recovery is slow and often incomplete.
Causes
Conditions resulting in the vitamin deficiency and its effects include chronic alcoholism and severe malnutrition. Alcoholism may be an indicator of poor nutrition, which in addition to inflammation of the stomach lining, causes thiamine deficiency. Other causes include dietary deficiencies, prolonged vomiting, eating disorders, or the effects of chemotherapy. It can also occur in pregnant women who have a form of extreme morning sickness known as hyperemesis gravidarum. Mercury poisoning can also lead to Korsakoff’s syndrome. It has also been caused by centipede (mukade) bites in Japan.
There is no specific treatment because the previous thiamine deficiency produces irreversible damage to the medial thalamic nuclei and mammillary bodies. Mammillary body atrophy may be visible on high-resolution MRI.
Prevention
The most effective method of preventing Korsakoff’s syndrome is to avoid B vitamin/thiamine deficiency. In Western nations the most common causes of such deficiency are alcoholism and weight disorders. In the U.S., government mandates to adding thiamine to alcoholic beverages have been blocked for this reason and also by political groups asserting that such supplementation would encourage alcohol use.
Case studies
A famous case study is recounted by Oliver Sacks in “The Lost Mariner” and “A Matter of Identity”, which can be found in The Man Who Mistook His Wife for a Hat. Other cases include German entertainer Harald Juhnke, artist Charles Blackman, and entertainer Graham Kennedy.
In popular culture
- Strangers is a play by Edward Einhorn based on the syndrome.
- In the Half-Life 2 mod Korsakovia, by thechineseroom, the player character Christopher is under treatment for Korsakoff’s Syndrome.
- In the television show House, season 1 episode “Histories,” Dr. House diagnoses a patient with Korsakoff’s syndrome after she gives different explanations for a sprained wrist to different interns who independently take her history.
- Internet comedy sketch group Derrick Comedy features a man with Korsakoff’s syndrome in their video “Progression of a Mad Hatter”.
- In the episode “Keeping the Faith” of the television show “Royal Pains” first aired on 06/17/10, Korsakoff’s syndrome is offered as a diagnosis for a female who had previously undergone a stomach reduction surgery.
- In the novel Now Wait for Last Year by Philip K. Dick, The main character’s wife is diagnosed with the syndrome after years of drug and alcohol abuse.
- It is probable that Boston Corbett, the man who shot John Wilkes Booth, suffered from Korsakoff’s syndrome later in life due to his pre-and-post war profession as a hatter, and his eventual madness.
- Davey Volner winner of the 81st Glascock Prize wrote a poem titled Korsakoff’s Syndrome
- Dr. Butz, the attending physician in the movie, “Critical Care” (1997) requests the etiology and symptoms of Korsakoff’s syndrome of his resident, Dr. Ernst.
Drug-induced amnesia
Drug-induced amnesia is amnesia caused by drugs. It may occur due to the use of recreational drugs such as alcohol, and it is used in surgery in order to make a patient forget painful or otherwise traumatic procedures.
Medical usage
Premedicants may be used to help a patient forget surgery or medical procedures, particularly those not performed under full anesthesia, or likely to be particularly traumatic. The drugs most commonly used for this purpose are a 2′-halogenated benzodiazepine such as midazolam or flunitrazepam is the drug of choice, although other strongly amnestic drugs such as propofol or scopolamine may also be used for this application. Memories of the short time frame in which the procedure was performed are permanently lost or at least substantially reduced, but once the drug wears off, memory is no longer affected.
Alcohol related
Alcohol can cause both long-term and short-term memory loss.
Electroconvulsive therapy and effects on memory
It is the purported effects of ECT on long-term memory that give rise to much of the concern surrounding its use. The acute effects of ECT can include amnesia, both retrograde (for events occurring before the treatment) and anterograde (for events occurring after the treatment). However, the vast majority of these effects are short lived. Memory loss and confusion are more pronounced with bilateral electrode placement rather than unilateral, and with outdated sine-wave rather than brief-pulse currents. The vast majority of modern treatment uses brief pulse currents. Research by Harold Sackeim has shown that excessive current causes more risk for memory loss, and using right-sided electrode placement may reduce verbal memory disturbance.
Retrograde amnesia is most marked for events occurring in the weeks or months before treatment, with one study showing that although some people lose memories from years prior to treatment, recovery of such memories was “virtually complete” by seven months post-treatment, with the only enduring loss being memories in the weeks and months prior to the treatment. Anterograde memory loss is usually limited to the time of treatment itself or shortly afterwards. In the weeks and months following ECT these memory problems gradually improve, but some people have persistent losses, especially with bilateral ECT. One published review summarizing the results of questionnaires about subjective memory loss found that between 29% and 55% of respondents believed they experienced long-lasting or permanent memory changes. In 2000, American psychiatrist Sarah Lisanby and colleagues found that bilateral ECT left patients with more persistently impaired memory of public events as compared to RUL ECT.
Some studies have found that patients are often unaware of cognitive deficits induced by ECT. For example, in June 2008, a Duke University study was published assessing the neuropsychological effects and attitudes in patients after ECT. Forty-six patients participated in the study, which involved neuropsychological and psychological testing before and after ECT. The study documented substantial cognitive impairment after ECT on a variety of memory tests, including “verbal memory for word lists and prose passages and visual memory of geometric designs.” The study further found that a significant number of patients believed that their memory had improved after ECT despite the fact that neuropsychological testing clearly showed the opposite. As stated by the researchers, “Indeed, there was a slight trend towards [patients reporting] improved memory functioning, despite the objective neuropsychological data indicating significantly lower recognition and delayed recall.” Based on their findings, the authors issued the following recommendation:
“When ECT is provided to adolescents, the potential impact of such cognitive changes should be discussed with the patients and their parents or guardians in terms of implications for not only the patient’s emotional functioning but cognitive functioning as well, particularly upon his or her academic performance. In summary, we argue that an individual cost-benefit analysis should be made in light of the implications of the potential benefits versus costs of ECT upon improving emotional functioning and the impact that potential memory changes may have on real-world functioning and quality of life.”
Severe memory loss from ECT is described in an autobiographical book, Doctors of Deception: What They Don’t Want You to Know about Shock Treatment.
Prosopamnesia
Prosopamnesia is a rare neuropsychological deficit defined by an inability to remember faces. It can be subdivided into two different types, including a ‘congenital’ and ‘acquired’ version.
Congenital (developmental) prosopamnesia involves an inborn difficulty in remembering faces, but having intact facial recognition and perception abilities. These abilities can be tested using the Cambridge Face Perception and Cambridge Facial Memory Test, available online. A case report of congenital prosopamnesia demonstrated a subject’s inability to neurologically “adapt” to images of faces using functional Magnetic Resonance Imaging (fMRI). The authors relate this deficiency to the brain’s inability to maintain a stable perception of the face long enough to encode it into long-term memory.
There is a case report of acquired prosopamnesia in which a subject experienced both retrograde and anterograde facial memory loss after a motorcycle-related head injury.
Prosopamnesia should not be confused with the similar condition prosopagnosia, which is characterized by a difficulty perceiving faces. An inability to “see” faces in such a manner will naturally be associated with prosopamnesia, as a facial memory trace cannot be formed without an ability to initially see the face.